A few weeks ago we were excited as NHS Hack Day visited Newcastle for the very first time.
As ever, we brought clinicians, patients, and other NHS staff together with developers, designers, researchers and others to share experiences, and spend a weekend working on short projects that address some of the frustrations and problems faced by patients and NHS staff every day.
After an initial session pitching potential project ideas to the group, the attendees gradually formed into teams and started work, exploring the spaces around the problems they’d chosen to work on, making new friends, and examining potential ways to address them.

You can see all of the teams that formed on the event page of the NHS Hack Day website, but a special mention here goes to a couple of our favourites:
Recording consent preferences
The “North Share” team spent much of the weekend exploring the thorny issues around consent, privacy and data sharing in the context of the NHS. Recent experience with a range of national and local projects suggests that there is plenty of work do be done in this area, and contributions in the form of tangible prototypes that help people to tell stories about and think through the issues involved are particularly helpful.
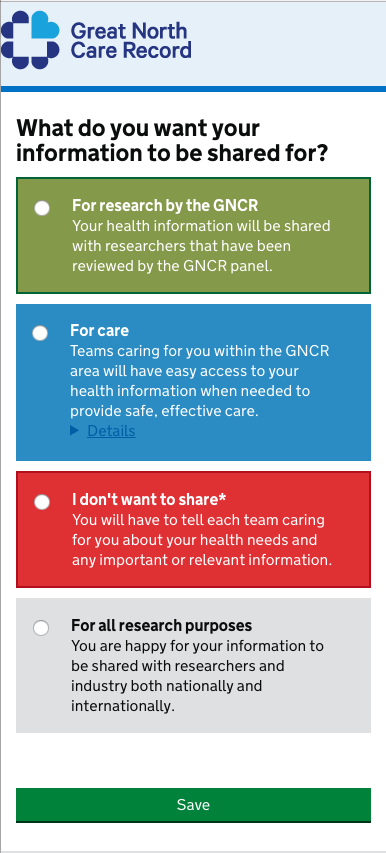
You can take the prototype they made for a spin yourself and see what you think - try asking questions like:
- do I understand what this means?
- what do I think this should do?
- what the consequences would be?
- how would I change this to make it better?
Managing consent, and doing the right thing around privacy and personal data is something we spend lots of time thinking about at Open Health Care, so it was great to see others in the community engaging with the issues in such a constructive, positive way.
Locating Community Dentistry
Highlighted on the NHS Hack Day mailing list beforehand was how hard it is for people with complex needs to locate appropriate community dental services via the NHS Choices website. (You’re likely to be able to find a general dental surgery, but no information about specialist services for people with complex medical comorbidities, physical disabilities, dementia etc)
Not for the first time, we find a situation where a lack of available complete, canonical data about the Physical NHS (the services on the ground across the country) makes it harder than is acceptable for patients to get the care they need.
At the event the team built a prototype of a service that would help people locate dental services appropriate for their situation.
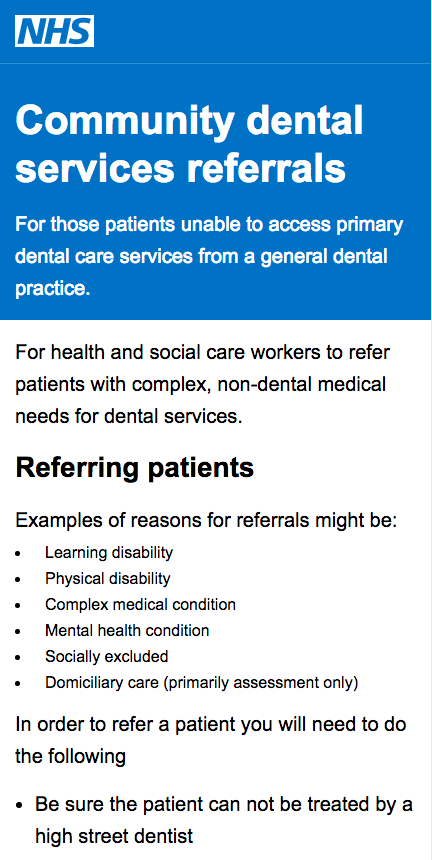
This prototype allows the team to tell the story of how the world should work for people trying to access dental services even though the data is unavailable (in fact, doesn’t exist).
One of the really interesting classes of hack day projects is the ones that go on to become campaigns on a particular topic - which is exactly what caught the eye with this one. This information is really something that should be rolled into the services developed by NHS Digital like NHS Choices, or the up-coming NHS.UK.
Having a (semi) working service to show people makes it much easier to tell the story of why this should exist, and helps to lobby the institutions who should be providing this data.
We’re sure this story isn’t over here and look forward to the time when these services are easy to locate.
Thanks and the future
Thanks to everyone who turned up over the weekend and helped to make it such a welcoming, friendly event. Particular thanks to the volunteers who helped make things run smoothly, and the sponsors without whom we wouldn’t be able to carry on running these events.
A particularly large thanks goes to Becky for leading the organization and cat-herding this time, and doing by far the lion’s share of dealing with suppliers, venue and sponsors.
If you want to come to a future NHS Hack Day then you can follow us on Twitter, or sign up to our mailing list and we’ll let you know as soon as we schedule the next one - likely early in 2017.
Read more